Tropical Medicine Institute: chronicles of the collapse

Español // English

Thursday
The blood drop became clear as the bioanalyst adjusted the microscope. Tailed parasites wiggled their way outside the red blood cells. He turned the eyepiece again. The parasites had a “C” shape. He was not expecting that result. The test sought to confirm a malaria diagnosis, but that blood was contaminated with Trypanosoma cruzi. The patient had Chagas disease. She was a nine year old girl living in Chacao. The bioanalyst was not aware of any contagion in Caracas’ urbanized heart.
The kissing bug (chipo) infected with Trypanosoma cruzi transmits Chagas disease. It stings and drops feces full of parasites. When a stung person scratches their skin, the parasite penetrates it reaching the bloodstream and traveling to the heart. A second contagion possibility is less common but more aggressive: ingesting food or drink contaminated with the kissing bug’s infected feces.
The bioanalyst knew the parasite well. He studied it at the Parasitology course of the Tropical Medicine Institute (IMT) of the Universidad Central de Venezuela (UCV) (Central University of Venezuela). He had seen it many times in the Hospital Universitario de Caracas (University Hospital of Caracas) laboratory. That is why he knew he faced an emergency. He reached the pediatrician and asked if the patient showed signs of a chipo’s bite. After several days of high fever, the girl had asked for a medical appointment. It was December 2007. Her face was swollen and she could not get up from bed. If she was suffering an acute stage of the disease and there was no apparent point of contact with the kissing bug, other similar cases were possible. They needed help.
Chagas disease affects seven million people worldwide. In three out of ten patients, it causes heart disease according to the World Health Organization (WHO). Sometimes it attacks the esophagus and the colon. In other cases, it deteriorates neurological functions as well. As it is a stigmatized by its relationship with poverty, it is a forgotten disease, according to the WHO. If the parasite reached the girl’s heart, she was at risk of losing her life.
The pediatrician and the bioanalyst exited the Hospital Universitario, walked a block inside the UCV and delivered the results to the IMT.
–I saw a Trypanosoma. We have Chagas in Chacao –said the bioanalyst.
Doctor Belkisyoslé de Noya put on her glasses and read the tests’ results. She ran the Immunology Section, the laboratory specialized in the diagnosis of Chagas disease. She began studying medicine at the UCV at 16 years old, in the late 60s. Right after graduating, she headed to New Orleans to study Medical Parasitology at the University of Tulane, with a scholarship from Venezuela’s National Council for Scientific and Technological Investigations. In 1980 she started teaching at the IMT. She has been running the institute since 2016.
Noya was fascinated by parasites since undergrad, when she was a student of Doctor Félix Pifano´s Tropical Medicine class. After flying over the UCV campus with former venezuelan president Rómulo Betancourt to choose the location of the Institute, Pifano founded the IMT in 1947. He requested the building to be placed beside the Jardín Botánico de Caracas (Caracas’ Botanical Garden).
Three endemic diseases afflicted Venezuelans in the mid-40s: malaria, hookworm disease and Chagas disease. The Anopheles mosquito transmitted malaria. The Necator americanus parasite’s larvae entered the body through the soles of people's feet and filled the belly with worms (hookworms). The kissing bug’s bite spread Chagas disease. Pifano participated in a campaign directed by Arnoldo Gabaldón to eradicate all three of them. They sprayed DDT and killed Anopheles, spread messages encouraging Venezuelans to wear shoes and fought the use of palm and adobe to build housing. Adobe and palm trees were the usual nesting place for kissing bugs. Pifano took charge of Yaracuy state, where he had worked as a rural doctor. Thanks to this policy, Venezuela became the first country in the world to get rid of malaria. During the 43 years that Pifano directed the IMT, he bred and studied the Rhodnius prolixus, the most common kissing bug type in South America’s northern region. For more than 70 years, the institute led the diagnostic, treatment, prevention and investigation of tropical diseases in Venezuela.
Friday
Noya met with the mother and grandmother of the Chagas patient. They told her the child had a dog. The doctor thought that maybe the dog carried the parasite. On Monday, they would take a sample from the animal. In Caracas, the Panstrongylus geniculatus predominated, an kissing bug that had adapted to the city and no longer looked for palm or adobe, but for light sources such as light bulbs, TV screens or computer screens. It lodged in dogs, cats and rats.
The mother and grandmother were thankful for the doctor’s explanations. They were convinced everything would turn out fine. While Noya dispatched them at the door of her practice, the grandmother commented that that morning she had run into a teacher of the Escuela Municipal Andrés Bello de Chacao (Andrés Bello Municipal School of Chacao), where her granddaughter studied. She was at the hospital too. She had a fever and her face was swollen. She said that other colleagues had the same symptoms. Noya became alarmed. They were not facing an isolated case. They had to find all infected people before it was too late.
The Tropical Medicine Institute was founded in 1947 inside the Central University of Venezuela.
The Tropical Medicine Institute was founded in 1947 inside the Central University of Venezuela.
Doctors within the Institute research new diagnostics methods for tropical diseases.
Doctors within the Institute research new diagnostics methods for tropical diseases.
Doctor Belkisyoslé Noya teaches class during a patient consultation. She heads the Tropical Medicine Institute since 2016.
Doctor Belkisyoslé Noya teaches class during a patient consultation. She heads the Tropical Medicine Institute since 2016.
Isía contracted Chagas disease in Chacao when she was only five years old.
Isía contracted Chagas disease in Chacao when she was only five years old.
Biological samples from tropical disease patients are stored inside refrigerators at the institute.
Biological samples from tropical disease patients are stored inside refrigerators at the institute.
The doctor went to the Hospital Universitario and confirmed that the teacher was infected with Trypanosoma cruzi. Just like the girl, she had no bite marks. Noya called the school and talked to the principal, Graciela Borrero. After working 20 years as a PE teacher, that year was her first as a school principal. Noya explained that two of the members of the school’s community had Chagas disease. She told her that the only common ground between the patients was the school. Borrero confirmed that several students missed class the previous week. Some teachers had asked for a medical leave. They had fever, headaches and looked swollen. Noya warned that they needed to start an epidemiological inquiry as soon as possible.
Monday
Noya arrived at the school accompanied by IMT doctors and bioanalysts to take blood samples. Borrero called a meeting to inform parents about the epidemiological investigation. Some were distressed, others offered help. A mother asked why the IMT doctors said their children were sick if they had not examined them. She preferred to consult her personal pediatrician. When they heard there was a teacher hospitalized at the Hospital Universitario, various colleagues asked their blood samples to take precedence. Borrero did not comply. The children came first.
Tuesday
A student of the “B” section of preschool had a pericardial effusion. He was five years old. He died.
Isía studied in section “A”, she was also 5 years old when she got infected with the Chagas disease. Ernisa Borrero, her mother, took her to various pediatricians and none were able to provide a diagnosis. Nothing calmed her fever or her swollen throat. Isía cried so much that Ernisa was losing her calm. She was a nurse. A doctor recommended that she give her daughter honey with resin oil to make the fever go down. Ernisa trusted the indications and prayed to her father, who passed away months before, not to take her away.
Wednesday
The phone rang at Ernisa’s house. It was Graciela, her sister, the principal of the school.
–Is Isía still sick? –asked Graciela.
–Her fever won’t go down –Ernisa answered.
–Bring her. We have two patients from the school who have Chagas disease. Some doctors are investigating how many children are infected.
–Chagas? That can’t be possible. That has no cure.
–A child from preschool died yesterday –said Graciela. She started crying.
Thursday and Friday
Noya and her team moved to the IMT. They took blood samples from a thousand patients that week of December 2007. Their cars were parked night and day at the institute’s gates, guarded by watchmen. They took turns to eat, so they would not interrupt the processing of the ELISA test, a diagnostic method designed to identify antibodies against the Trypanosoma cruzi and other diseases in the blood of each patient. If the antibodies’ concentration surpassed 0,230 absorbance units, the patient was infected.
The investigators categorized the patients. Group 1: asymptomatic patients. Group 2: patients with mild or moderate symptoms. Group 3: very sick patients, at home or hospitalized. They stored the information in a database: name and last name, age, gender, diagnostic, clinical manifestations, hospitalized or not, place of hospitalization. As they got results, they printed out the diagnostic of each patient in pages that had letterheads of the institute and the values obtained through the tests.
Doctor Noya worked with her husband, Oscar Noya, also a medical parasitologist; pediatrician Raiza Ruiz-Guevara, biologist Zoraida Díaz Bello and bioanalyst Luciano Mauriello. Diagnosing all patients was so urgent that they spent nights at the laboratory.
The following week
They detected 103 infected people. 77 were children and 26 were adults. The infection was mild or moderate in half the cases. The rest were severe. A lot of them were at risk of suffering a pericardial effusion, like the preschool student. They had never treated so many Chagas disease patients at the same time. They had never identified a contagion of this magnitude in the country, much less in Caracas. They were in front of the first oral outbreak of the Chagas disease registered in Venezuela.
In the first phase of the oral infection, there are no symptoms. The Trypanosoma cruzi reproduces itself in the stomach and spreads to the rest of the organism. The parasite circulates freely; the organism still has no antibodies to fight it. It travels through blood, it lodges in the muscles of the heart and swells it. Everything can happen in eight days.
A diabetic child that never ate from the school menu turned out to be Chagas-free in the tests. That strengthened the suspicion that the infected patients ate or drank something distributed at the school that was contaminated. The challenge was to discover how they were infected.
The Andrés Bello Municipal School distributed breakfast, lunch and snacks to 130 students in 2007. Most of them were preschoolers and first, second and third grade students. They served ham and cheese arepas, sandwiches, oatmeal, pabellón or spaghetti with bolognese sauce or chicken, cakes and cookies, accompanied by chicha or natural fruit juice. When there were leftover drinks, they gave them to the teachers. Everything was made outside of the school; there was no kitchen on school grounds.
To identify the infected food, Noya and her team asked the patients what they had ingested. They discarded the food and the drinks remained. Not everyone had oatmeal or chicha. They examined the list of fruit juice until they discovered the only one that was ingested by all 103 infected people: guava juice. Doctor Noya presented the hypothesis that the infection was spread through that juice. If they found a kissing bug where it was made, it would confirm the origin of the contagion.
The Department of Health sent a few inspectors to El Tamarindo slums, at the north of Caracas. The woman who made the juice lived in a half-built brick house, blocks away from the Vargas Hospital. They found no kissing bugs. Doctor Noya entrusted a second attempt to investigator Matías Reyes, from the IMT. He was a biologist with a PhD in entomology and ecology in the Science Department of the UCV. He studied the life cycle of the insects and their relationship with humans and the environment. He bred mosquitoes, flies, cockroaches and kissing bugs at the Medical Entomology section of the IMT. He inaugurated the department. He designed the lab’s furniture where he worked, and supervised the carpenter that installed them, in a unit behind the institute’s main building. Sometimes he slept at the laboratory to monitor his experiments.
Doctors analyzed blood tests from patients of the Chagas Chacao outbreak to isolate the parasites.
Doctors analyzed blood tests from patients of the Chagas Chacao outbreak to isolate the parasites.
Professor Reyes visited the house, saw some dogs and asked where they slept. He assumed he was looking for a Panstrongylus geniculatus, Caracas’ most common kissing bug. He was pointed to a corner. There was a planter. He found a live kissing bug under the planter that allowed the confirmation of the hypothesis of the IMT medical team: the guava juice had been the vehicle for the infection. A few meters away, there was a glassless window behind the kitchen sink. The woman who made the juice told Reyes that she boiled the guava fruit at night and put the pot in front of the window without a lid. There was a lit light bulb above the pot.
The owner of a nearby bodega where the juice was prepared offered her business as a collection center for kissing bug. The following days, neighbors picked up a kissing bugs they found at home as instructed by Reyes: open a matchbox, place it over the insect, close it when the bug was underneath, write down the date, time and place where it was caught, and the contact information of the person who caught it, and take it to the IMT.
As soon as the patient’s treatment started, the institute’s database began to grow. The investigators added rows to register tests: blood tests, X rays, physical evaluations, electrocardiograms. They took pictures to document the effects of the disease on children and adults. They assigned a mouse to each patient in the lab where animals are bred for experimentation, the bioterium. They had the patients’ names. They were inoculated with the infected blood. After 11 days, they performed punctures to the heart muscles of the mice. They planted the blood in growing mediums and isolated the parasites. They identified where each patient’s infection was located and they created antigens to trigger immune responses. They treated the patients with Nifurtimox and Benznidazol, the only two medicines, antiquated and toxic, that existed to combat Chagas disease.
Daireth Juárez had a fever, a rash and pain on her back. She was 7 years old when she became infected. Her heart swelled. Salud Chacao, the public health system for inhabitants of Caracas’ municipality, Chacao, gave her a heart rate monitor to register the activity of her heart for 24 hours. The school donated batteries for the devices. She was given treatment for three months. Her mom mixed her medicine with peach juice, otherwise it was undrinkable. She was nauseous all the time. She lost weight. Six months after, the tests were done again. The parasite was still active. The treatment began again.
A decade later
Noya and her team monitored the evolution of the Chacao patients during the following years. They called them in for consultations to carry out annual controls at the IMT. They published articles in national and international scientific magazines about the first recorded oral Chagas outbreak in Venezuela.
A March Monday in 2016, doctor Noya received a call from the institute. She was at a scientific congress in Spain. That weekend someone had broken into the Immunology laboratory by beating down its door and stolen seven computers that stored the Chacao patients’ information. Anything that was not shared through pen drive devices or via e-mail, was lost.
Daireth Juárez had a fever, rash and back pain. She was seven years old when she became infected with Chagas disease.
Daireth Juárez had a fever, rash and back pain. She was seven years old when she became infected with Chagas disease.
Doctors from the Tropical Medicine Institute have monitored the Chagas Chacao patients for ten years.
Doctors from the Tropical Medicine Institute have monitored the Chagas Chacao patients for ten years.
Robbers violently destroyed the institute´s doors.
Robbers violently destroyed the institute´s doors.
The robbery of electric wiring affects the supply of electricity within the institute.
The robbery of electric wiring affects the supply of electricity within the institute.
Some laboratories do not have water supply because the piping was stolen.
Some laboratories do not have water supply because the piping was stolen.
The bioterium, where animals for experimenting are raised, is the most severely affected department of the institute.
The bioterium, where animals for experimenting are raised, is the most severely affected department of the institute.
Original infrastructure of the Tropical Institute have been intervened to reinforce security.
Original insfrastructure of the Tropical Institute have been intervened to reinforce security.
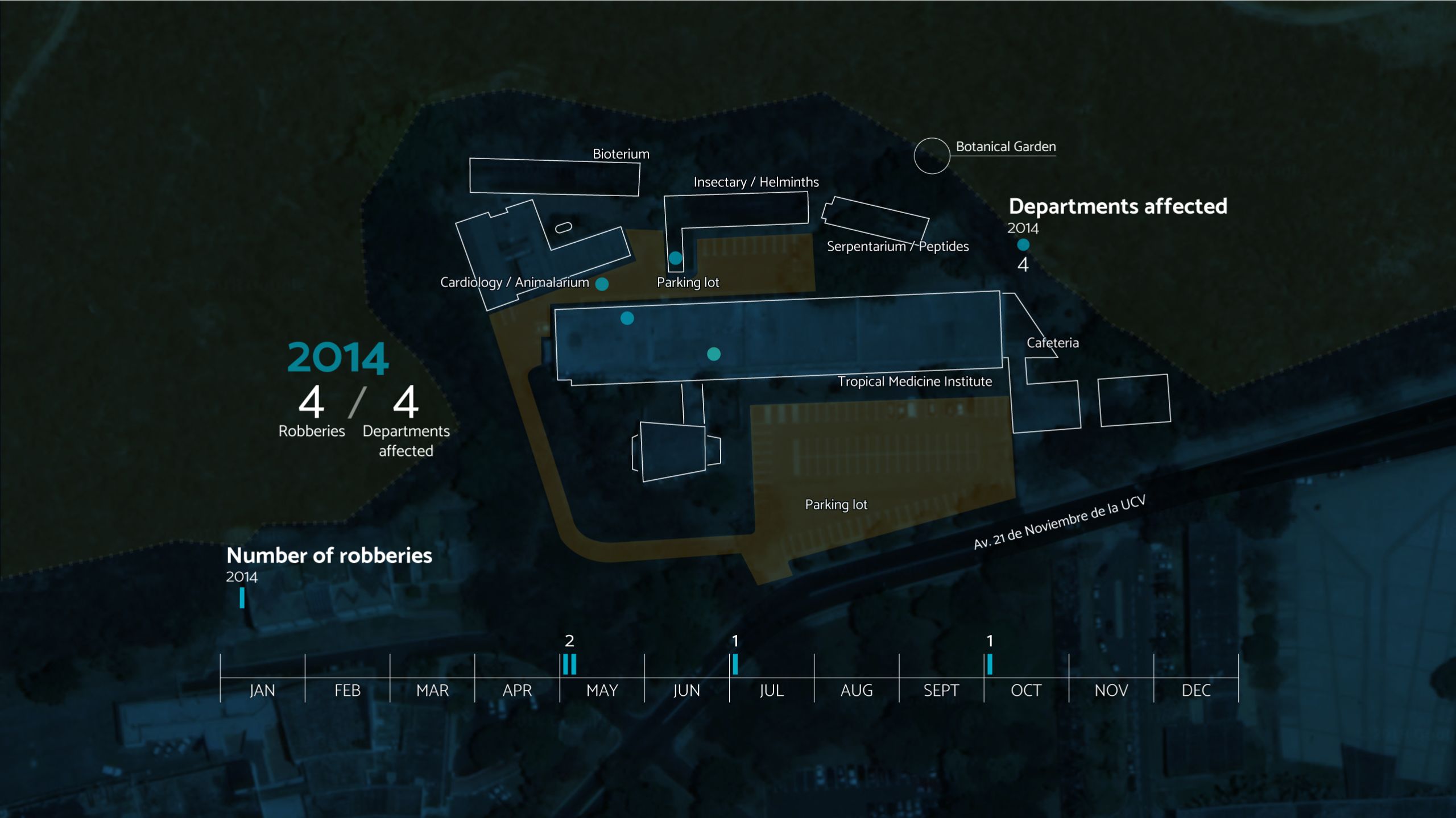
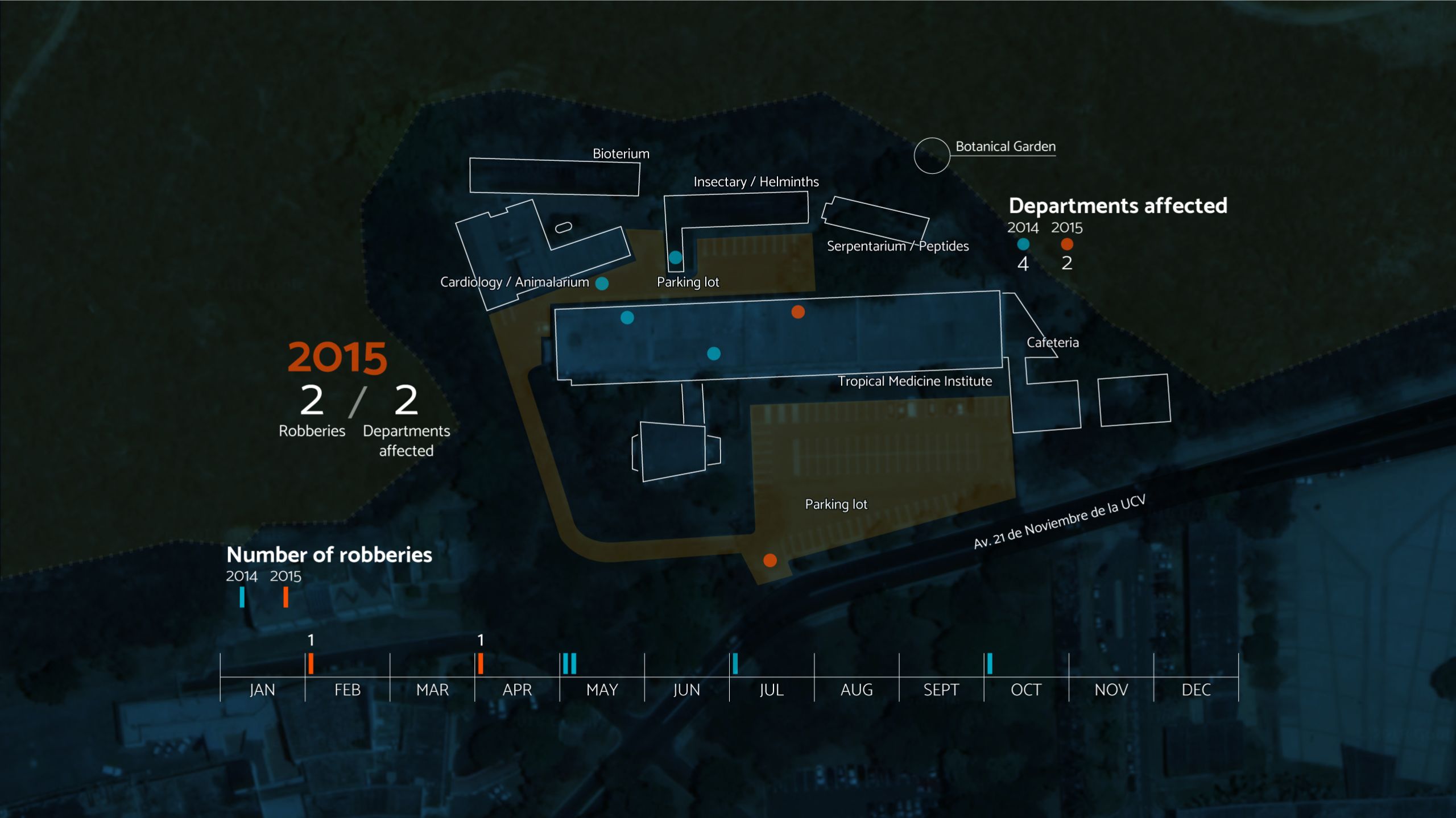
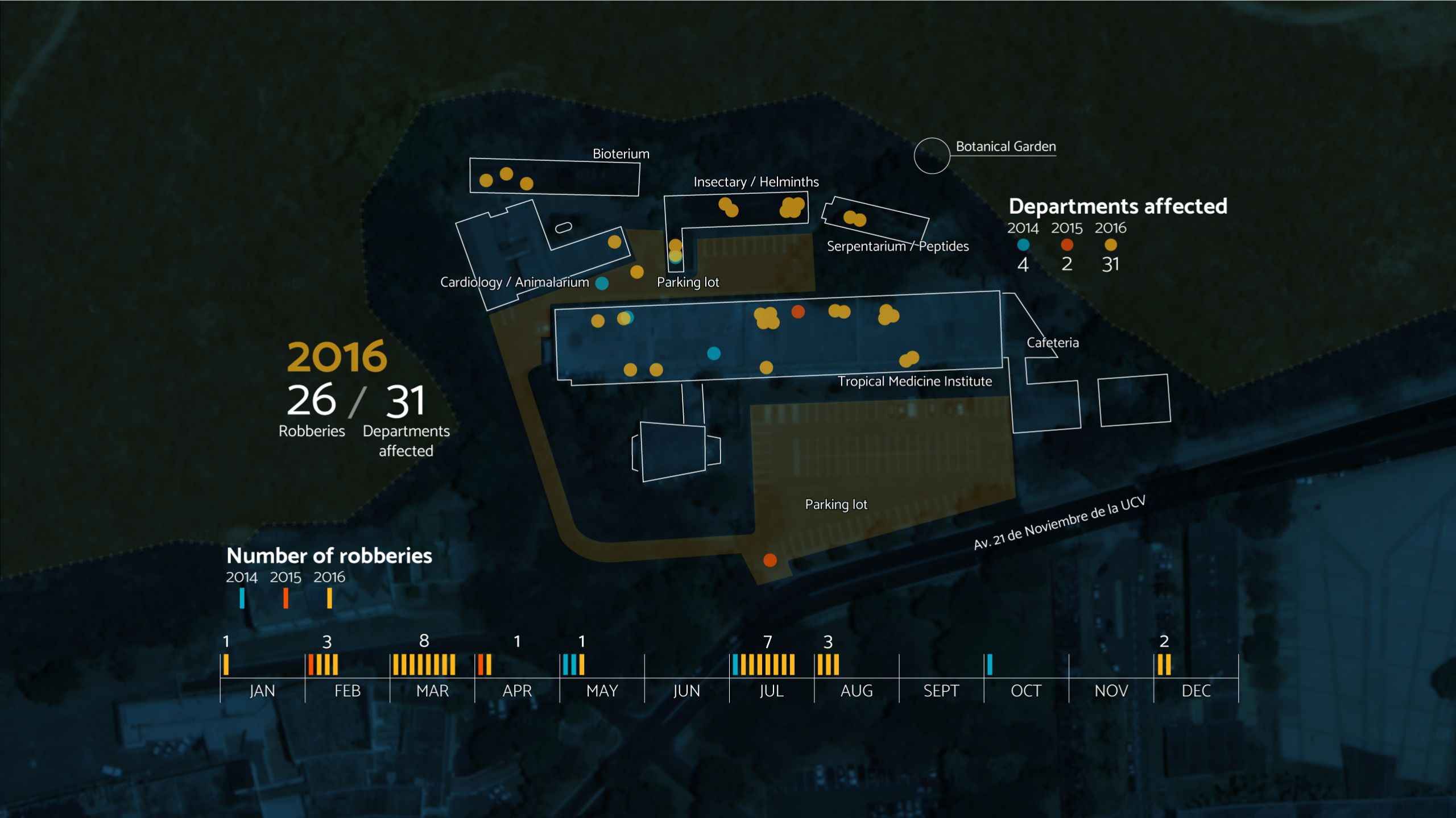
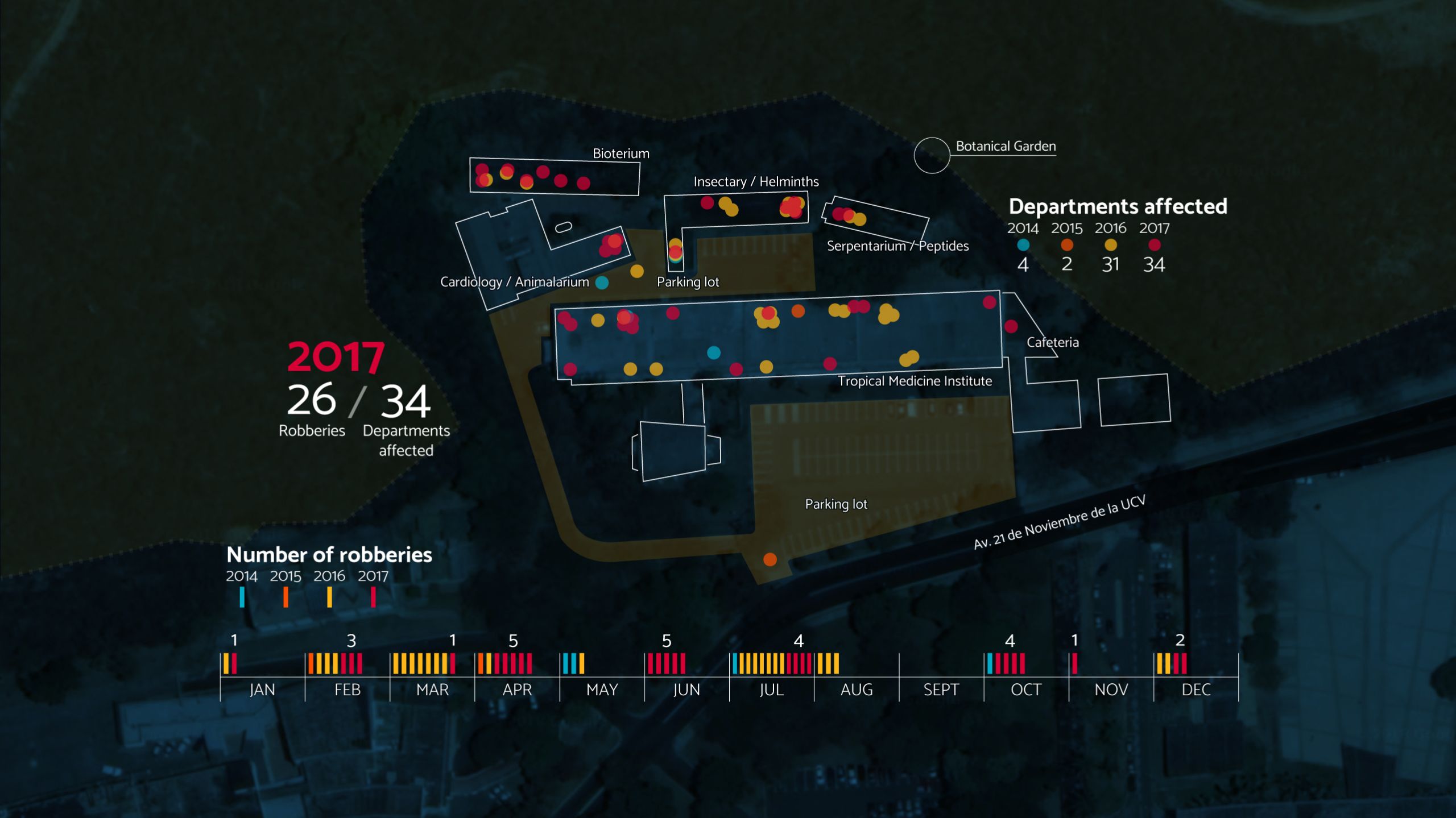
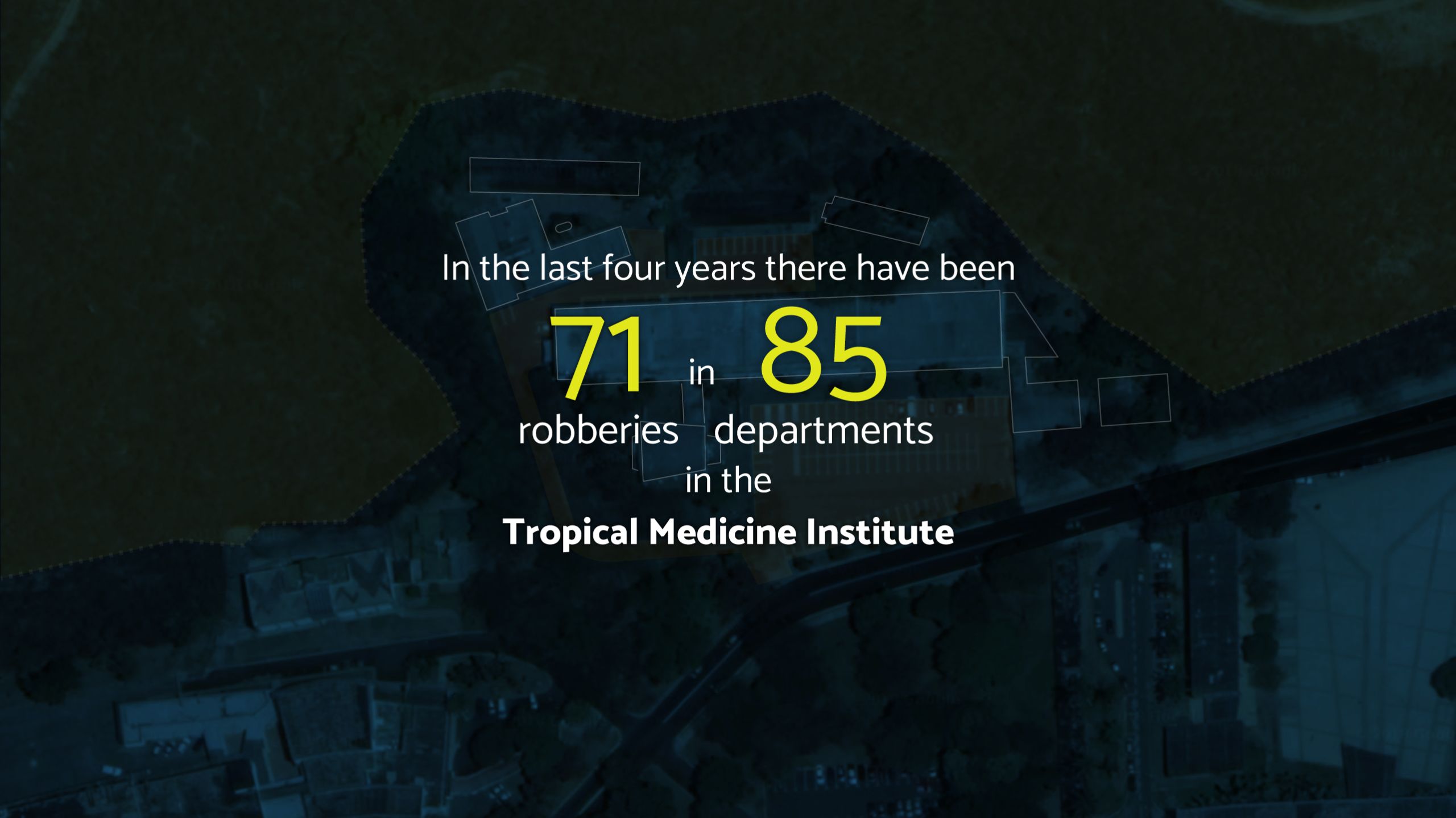
The IMT was robbed 71 times from May 2014 to April 2018. Doctor Noya registers what was lost in each robbery and the number of reports filed at the Cuerpo de Investigaciones Científicas, Penales y Criminalísticas (Scientific, Penal and Criminalistics Body of Investigation) in a database.
They have taken microscopes and toilet bowls. The IMT bought security doors with resources that could have been destined for investigation projects. Some doors are still wood, as originally designed by Carlos Raúl Villanueva. Others were replaced by bars and padlocks. Two of the teachers were mugged at the parking lot and had their cars, cell phones and wallets stolen. After class, scientists used to arrive at the laboratories at 5:00pm and work until 8:00pm. Now they leave at 4:00pm and they do it in groups.
One day, Professor Reyes arrived at the Medical Entomology laboratory to find that the fridges storing the reagents were gone. The coffee maker was also gone. Another day, the field investigation instruments were gone: a pH-meter, an altimeter, compasses, GPS devices, boots. Another day, they took the running water’s pipes. They also ripped out the electrical wiring and the laboratory was left in the dark, as were the Biohelmintiasis and Cardiology sections, and the Centro de Análisis de Imágenes Biomédicas Computarizadas (Biomedical Computerized Images Analysis Center) and the bioterium. The building behind the IMT does not have electricity since last year.
On May first of 2018 the institute was left without internet. They stole 120 meters of wiring from the Escuela de Medicina Luis Razetti (Luis Razetti Medical School), where the node that supplies internet connection for 11 dependencies of the UCV is located, most of them dedicated to health sciences: the IMT, the Instituto Nacional de Higiene (National Hygiene Institute), the Instituto Anatómico (Anatomical Institute), the Immunology one, the Servicio de Oncología (Oncology Service), the Decanato de la Facultad de Medicina (Deanery of the Medical Faculty), the Escuela de Medicina (Medical School), the Pharmaceutics and Odontology faculties, the Transship building, and the Organización de Bienestar Estudiantil (Student’s Wellbeing Organization). During several weeks, there was internet only from 8 to 11 in the morning. The UCV became a quarry of stolen copper to resell in the black market.
The Medical Entomology laboratory became dark and hot. They took the air conditioning units. As the lighting and temperature changes do not affect insects, there are glass containers and buckets filled with mosquitoes, flukes, roaches and kissing bugs. One of them stores the grandsons of the Rhodnius prolixus that Pifano bred. They are pure breed, useful for genetic testing. In the year 2000, the Environment Ministry qualified the biological collection of live animals of the IMT as the best in Caracas.
The flutter of bug’s wings can be heard as a postgraduate student makes a presentation from his personal computer. He charged its battery at home so he could have battery life to show all the slides in his dissertation presentation. The doctor can walk through the laboratory with his eyes closed. He knows the contents of all the jars and the advances of all experiments by heart.
When a company asks to certify the quality of a pesticide, the Medical Entomology laboratory of the IMT tests it on 200 or 400 cockroaches fed with dog food that contains 22% protein. It cannot have less than that. When the insects meant for experiments are weak, there is a risk of error in the sampling, risking poor quality pesticides to be certified. Sometimes the investigators pay for the dog food out of their own pocket.
After the delinquents killed five of the eight dogs that guarded the bioterium, it became the most robbed section of the institute. Jeferson Muñoz was breeding 250 mice for Chagas disease and toxoplasmosis tests in 2012. Six years later, two mice meant for diagnostics remain. A grey cat peeps inside the laboratories that still maintain some activity. Once, the thieves took –or freed- 50 mice that Jeferson infected with Trypanosoma cruzi for an investigation. He supposes the plastic cages appeared valuable for the robbers. He avoids imagining those 50 mice, loose in the tall grass that connects the IMT with the Botanical Garden and the La Charneca slum, filled with people potentially infected with Chagas disease.
In the laboratory next door, the Mycology one, they broke the shelves that stored spores carefully grown for years. Since it was highly contagious fungi, the Firefighters and the Brigada de Control de Emergencias del Instituto Nacional de Higiene (Emergency Control Brigade of the National Institute of Hygiene) had to seal the area, isolate it and decontaminate it.
The bioterium of the IMT can’t raise mice. In Venezuela, rat food has not been produced since 2017. It’s the ideal nourishment to meet the standards that experimentations need, according to international protocols. The capacity for diagnosis and investigation of the institute collapses without mice. The TORCH test is no longer carried out to check if pregnant women have toxoplasmosis, rubella, cytomegalovirus, herpes or hepatitis. There are only reagents to detect toxoplasmosis and pieces of paper to deliver the results, handwritten. The letter-headed sheets have run out, as has the ink to print the results.
In June 2018, the Panamerican Health Organization reported historic peaks of malaria and diphtheria contagion in Venezuela in 2016 and 2017. The IMT’s investigators have the experience and the expertise to lead an emergency national campaign that stops the transmission of these tropical diseases, according to Rafael Orihuela, deputy director of the IMT for ten years and former Health minister.
The IMT budget assigned by the university is not enough to buy detergent for cleaning its common areas. Alumni and professors had to use surgical gloves to mow the lawns in 2017. That was how they celebrated the 70th anniversary of the institute’s foundation.
The National Master in Parasitology was closed, for the first time in two decades, in 2017.
The National Master in Parasitology was closed, for the first time in two decades, in 2017.
The National Master Program of Parasitology was closed in 2017. For the first time in 21 years, the institution did not have funds to run the experiments that students have to carry out for their dissertations.
If there is a Chagas disease outbreak today as the one in Chacao, finding the “C” shaped tailed parasites outside of the red blood cells at the IMT, would not be possible. The Immunology lab has not had any electricity since last year. The wires were stolen. Out of the four microscopes available, three were robbed. Since no mice are bred at the bioterium, the investigators would have to buy them at the National Institute of Hygiene, that doesn’t have any rat food either. Eleven years later, they could not detect, diagnose and treat a hundred patients infected with the Chagas disease in a week.
Another investigator migrated. In the halls of the Tropical Medicine Institute, professors lament between themselves. Some of them started the paperwork to leave. Others trust the country’s situation will change; they will wait a few months to see what happens. Doctor Noya has family in Spain. Every time she analyzes this dilemma, she reaches the same conclusion: “What am I going to do in Spain? Here, I can heal people. I am needed here. I was born here and I want to die here”.
***



Credits
Editor in Chief: Ángel Alayón and Oscar Marcano
Deputy Managing Editor, Investigative Department: Valentina Oropeza
Photography editor: Roberto Mata
Head of Design: John Fuentes
Head of Innovation: Helena Carpio
Infographics: John Fuentes, Maria Fernanda Callejón
Text: Valentina Oropeza
Translation: Gabriela Delgado, Helena Carpio y Diego Marcano
Photography: Diego Vallenilla
Digital product manager: Helena Carpio
Social media: Salvador Benasayag
Caracas. Wednesday july 18, 2018



















